Psychiatric documentation is a crucial aspect of providing effective patient care, as it serves as a comprehensive record of the patient’s condition, progress, and treatment. To ensure accuracy, consistency, and efficiency in documentation, psychiatric documentation templates have become an invaluable tool for mental health professionals.
In this guide, we will delve into the significance of psychiatric documentation templates, explore the various types available, and discuss key elements that should be included. We will also provide best practices for using these templates effectively, examine technological advancements that are enhancing documentation, and showcase examples of commonly used templates. By leveraging the power of psychiatric documentation templates, mental health professionals can streamline documentation, improve accuracy, and ultimately provide better care for their patients.
Definition and Purpose of Psychiatric Documentation Templates
Yo, let’s get real about psychiatric documentation templates. They’re like the secret sauce for keeping your patient records lit and accurate. Standardization is key in psychiatry, bruv. It helps us track symptoms, treatments, and progress over time. And when you’ve got pre-designed templates, it’s like having a cheat code for writing up your notes.
Think about it, fam. Templates streamline the process, making it a breeze to record all the important deets. No more wasting time trying to figure out what to write or how to structure your notes. Plus, they help you stay on track and avoid missing any crucial information. So, basically, templates are your homies when it comes to keeping your documentation on point.
Benefits of Using Templates
- Streamline documentation, making it quicker and easier.
- Improve accuracy by providing a consistent structure.
- Ensure all relevant information is captured.
- Facilitate communication between healthcare professionals.
- Meet regulatory and legal requirements.
Types of Psychiatric Documentation Templates
Psychiatric documentation templates provide a structured framework for recording and organizing patient information, ensuring consistency and accuracy in clinical practice. These templates vary in purpose and scope, catering to specific aspects of psychiatric assessment and treatment.
Commonly used psychiatric documentation templates include:
- Intake Assessment Template: Captures patient demographics, presenting problems, history of illness, and treatment goals.
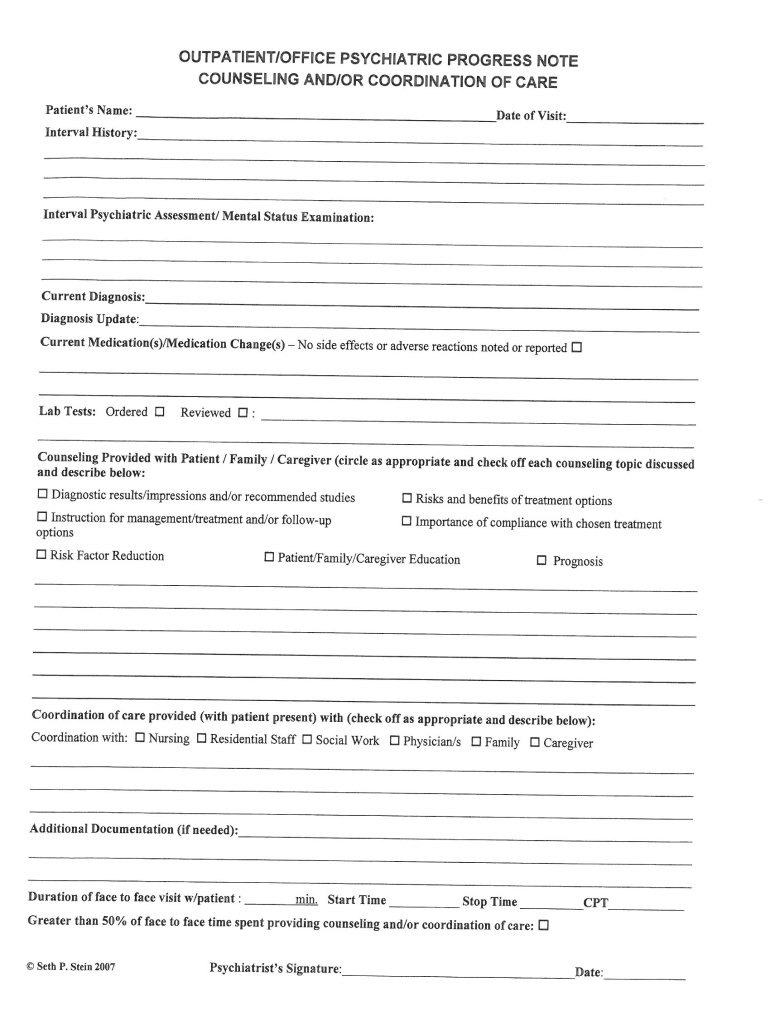
- Progress Note Template: Documents patient progress, treatment interventions, and any changes in symptoms or functioning.
- Discharge Summary Template: Summarizes the patient’s hospital stay, including diagnosis, treatment provided, and recommendations for follow-up care.
- Medication Management Template: Tracks medication prescriptions, dosage, side effects, and patient adherence.
- Consultation Note Template: Records consultations with other healthcare professionals, providing a summary of the patient’s condition and recommendations.
- Psychological Assessment Report Template: Documents the results of psychological testing, including intelligence, personality, and neurocognitive functioning.
- Forensic Evaluation Report Template: Provides an evaluation of a patient’s mental state for legal purposes, such as competency to stand trial or criminal responsibility.
Advantages and Limitations of Different Template Formats
Psychiatric documentation templates come in various formats, each with its advantages and limitations:
- Paper-Based Templates: Offer portability and flexibility, allowing clinicians to document information offline.
- Electronic Health Record (EHR) Templates: Integrated into EHR systems, enabling easy access, sharing, and data analysis.
- Web-Based Templates: Accessible from any device with internet access, facilitating remote documentation.
The choice of template format depends on factors such as clinician preference, practice setting, and patient needs.
Key Elements of Psychiatric Documentation Templates
Psychiatric documentation templates are essential for capturing and organizing patient information. They provide a structured framework for documenting symptoms, diagnoses, treatment plans, and progress over time. To ensure the accuracy and completeness of documentation, it’s crucial to include key elements in these templates.
Subjective and Objective Data
Psychiatric documentation should include both subjective and objective data. Subjective data refers to the patient’s self-reported experiences, feelings, and thoughts. Objective data includes observable signs, symptoms, and behaviors. Capturing both types of data provides a comprehensive understanding of the patient’s condition.
Structured Questions
Structured questions can help clinicians gather specific and consistent information from patients. These questions should be clear, concise, and cover relevant aspects of the patient’s presentation. Using structured questions ensures that all necessary information is obtained and documented.
Rating Scales
Rating scales are standardized tools used to measure and quantify specific symptoms or behaviors. They provide a consistent way to track changes over time and assess the effectiveness of treatment. Common rating scales include the Hamilton Depression Rating Scale and the Brief Psychiatric Rating Scale.
Other Tools
In addition to structured questions and rating scales, other tools can enhance psychiatric documentation. These include:
- Checklists: Predefined lists of symptoms or behaviors that can be quickly checked off.
- Narrative Notes: Free-form text sections that allow clinicians to provide detailed descriptions and observations.
- Genograms: Diagrams that illustrate family relationships and patterns of illness.
By incorporating these key elements into psychiatric documentation templates, clinicians can create comprehensive and accurate records that support effective patient care and communication.
Best Practices for Using Psychiatric Documentation Templates
Psychiatric documentation templates are an essential tool for mental health professionals. They provide a structured and consistent way to record patient information, which can improve the quality of care and reduce the risk of errors. However, it is important to use templates effectively to get the most benefit from them.
Here are some best practices for using psychiatric documentation templates:
- Choose the right template for the patient. There are many different types of psychiatric documentation templates available, so it is important to choose one that is appropriate for the patient’s needs. For example, there are templates for initial evaluations, progress notes, and discharge summaries.
- Tailor the template to the specific patient population. Once you have chosen a template, you may need to tailor it to the specific patient population you are working with. For example, if you are working with children, you may need to add fields for developmental history and school information.
- Use the template consistently. Once you have chosen a template, it is important to use it consistently for all patients. This will help to ensure that the documentation is complete and accurate.
- Document all relevant information. The documentation should include all relevant information about the patient’s condition, including the patient’s symptoms, diagnosis, treatment plan, and progress.
- Be objective and factual. The documentation should be objective and factual. Avoid using judgmental or subjective language.
- Use clear and concise language. The documentation should be written in clear and concise language that is easy to understand.
- Review the documentation regularly. The documentation should be reviewed regularly to ensure that it is accurate and up to date.
By following these best practices, you can ensure that you are using psychiatric documentation templates effectively. This will help to improve the quality of care and reduce the risk of errors.
Technological Advancements in Psychiatric Documentation Templates
Technology has revolutionized psychiatric documentation, enhancing its efficiency and accuracy. Electronic health records (EHRs) have become the cornerstone of modern psychiatric practice, offering a digital platform for recording and managing patient information.
EHRs streamline documentation by providing pre-populated templates and automated prompts. This reduces the risk of errors and omissions, as clinicians can select from standardized options rather than manually entering data. Additionally, EHRs facilitate collaboration between healthcare professionals, allowing them to share patient records securely and efficiently.
Digital Tools
Beyond EHRs, various digital tools have emerged to further enhance psychiatric documentation. These include:
- Speech-to-text software: Transcribes spoken notes into digital text, saving time and reducing the burden of manual documentation.
- Mobile apps: Allow clinicians to access and update patient records on the go, ensuring timely and accurate documentation.
- Data analytics tools: Generate reports and insights from patient data, helping clinicians track progress and identify patterns.
These technological advancements have significantly improved the quality and efficiency of psychiatric documentation, enabling clinicians to provide better care to their patients.
Examples of Psychiatric Documentation Templates
Psychiatric documentation templates offer a standardized approach to documenting patient information, making it easier for clinicians to capture accurate and comprehensive data. These templates can be tailored to specific clinical scenarios, ensuring that all relevant information is captured.
Access and Utilization
Numerous resources provide access to a wide range of psychiatric documentation templates. Online repositories, professional organizations, and software vendors offer free and paid templates that can be easily downloaded and customized. These templates are typically available in various formats, including Word, PDF, and electronic health record (EHR) systems.
Template Showcase
Below is a table showcasing a variety of psychiatric documentation templates, each tailored to a specific clinical scenario:
| Template Name | Clinical Scenario | Access |
|—|—|—|
| Psychiatric Evaluation Template | Initial psychiatric evaluation | Online repositories, professional organizations |
| Treatment Plan Template | Development of a comprehensive treatment plan | Software vendors, EHR systems |
| Progress Note Template | Ongoing documentation of patient progress | EHR systems, online repositories |
| Discharge Summary Template | Summary of care provided and recommendations upon discharge | Professional organizations, software vendors |
| Crisis Assessment Template | Assessment of patients in acute crisis situations | Online repositories, professional organizations |
| Medication Management Template | Monitoring and tracking of medication adherence and effectiveness | EHR systems, software vendors |
By utilizing these templates, clinicians can streamline their documentation process, ensuring that all essential information is captured accurately and efficiently.
Frequently Asked Questions
What are the benefits of using psychiatric documentation templates?
Psychiatric documentation templates offer numerous benefits, including increased accuracy and consistency in documentation, reduced documentation time, improved organization and clarity, and enhanced compliance with legal and ethical standards.
What are the different types of psychiatric documentation templates available?
There are various types of psychiatric documentation templates available, each designed for a specific purpose. These include intake assessments, progress notes, treatment plans, discharge summaries, and risk assessments.
What are the key elements that should be included in a psychiatric documentation template?
Key elements that should be included in a psychiatric documentation template include patient demographics, presenting problem, history of present illness, mental status examination, diagnosis, treatment plan, and progress notes.
How can I ensure that my documentation meets legal and ethical standards?
To ensure that your documentation meets legal and ethical standards, it is important to use standardized templates, document all relevant information, maintain patient confidentiality, and obtain informed consent before releasing any documentation.